“Chronic inflammation has been linked to certain diseases such as heart disease or stroke, and may also lead to autoimmune disorders, such as rheumatoid arthritis and lupus. But a healthy diet and lifestyle can help keep inflammation under control.” – Jessie Szalay (source)
Inflammation is one of the most widely misunderstood health issues there is. While it is true that an out-of-whack immune system (which causes inflammation) can cause problems, inflammation – in and of itself – is not a bad thing. In fact, inflammation is an essential part of a healthy body and mind.
In this article, we’ll discuss the following:
- What inflammation is
- Why too much inflammation is a bad thing
- What causes inflammation complications
- The types of inflammation
- 7 signs that you are affected by abnormal inflammation (and what to do about it!)
What is inflammation?
Inflammation is an automatically-triggered immune system response that serves as a self-protection mechanism of the body. It is probable that inflammation has helped to heal and protect your body at some point. For example, if you’ve ever sustained any kind of injury – from minor to life-threatening – to any part of the body, the inflammatory response helped protect and heal the affected area.
Inflammation arises from physical reactions of the immune system due to infection, bodily injury, or illness.
What happens?
To help give a clearer (simplified) idea of what happens during inflammation, let’s use an everyday example. Let’s say that you were trying to slice a potato when you accidentally cut yourself with a small kitchen knife. The steps involved in a typical inflammation response in such a case would look something like this:
Step 1 (Hemostasis):
As soon as the edge of the knife penetrates the skin, the body instinctively knows that something is wrong and that the bleeding must be stopped. To achieve this, the body activates the blood clotting system by delivering tiny, disk-shaped cell fragments called platelets to the affected area. An enzyme in platelets, called thrombin, creates a mesh-like substance that clots the blood and eventually stops the bleeding.
Step 2 (Defensive phase):
Following hemostasis, neutrophils – a class of white blood cells – target any foreign invaders like bacteria. Neutrophils work to eliminate bacteria and begin removing any debris. After between 24 to 48 hours, specialized cells called macrophages arrive and secrete chemicals (e.g. proteins, growth factors) to signal that the area is ready for tissue repair. It is during this four- to six-day “cleaning” period when the inflammation symptoms of heat, pain, redness, and swelling peak.
Step 3 (Proliferation phase):
After the wound is clean, the body begins the process of filling and covering the cut. Connective tissue settles around the wound and forms new blood vessels, which causes the areas of separated skin caused by the cut to merge. Epithelial cells “hop” from the separated areas until the cut is fully covered by new skin tissue.
Step 4 (Maturation phase):
The shiny new skin tissue now covering the paper cut needs to mature. Collagen tissues work to increase “tensile strength,” not only increasing the skin’s toughness, but also enhancing flexibility. Throughout this dynamic process, the new skin tissue will continue to remodel and mature for up to four months. (1)
Types of inflammation
There are two types of inflammation, acute and chronic, categorized according to the state of the immune system and longevity of the immune response.
Acute Inflammation
Acute inflammation begins quickly and exacerbates in severity over a short period. The symptoms and signs of acute inflammation are comparatively shorter than that of chronic inflammation, lasting from a couple of days to approximately four weeks. Medical conditions associated with acute inflammation include: acute bronchitis, appendicitis, cutting or scratching of the skin, dermatitis, ingrown toenail, infective meningitis, sore throat due to cold or flu, sinusitis, and tonsillitis. Certain physical trauma, as well as high-intensity exercise, can result in acute inflammation. (2)
The symptoms of acute inflammation around areas of the skin form the acronym PRISH:
- Pain: The nerve endings of inflamed areas are very sensitive, especially early on.
- Redness: Wounds that are inflamed are red due to the increased blood flow into the capillaries.
- Immobile: Inflammation may also cause loss of movement in certain areas of the body.
- Swelling: Additionally, fluid accumulation leads to a swollen appearance.
- Heat: A sense of heat arises because of the higher-than-normal levels of blood surrounding the affected area. (2)
Chronic inflammation is generally linked to a long-term medical condition, such as most forms of arthritis and some forms of cancer. Acute and chronic inflammation differ regarding cause, onset, period, and outcomes (see table below.)
Other conditions and diseases marked by chronic inflammation include asthma, hepatitis, inflammatory bowel diseases (e.g. Chron’s disease), peptic ulcer, rheumatoid arthritis, periodontitis, sinusitis, and tuberculosis.
| Inflammation Type | Acute | Chronic |
|
Cause |
Bacteria or injury |
Resistant pathogens from infections (e.g., viruses), abnormal immune response. |
|
Onset |
Rapid |
Eventual |
|
Period |
Days |
Months or years |
|
Outcomes |
Healing through natural or medicinal intervention; becomes an abscess, or becomes chronic | Death of affected tissue and scarring of connective tissue |
(source)
7 Signs of “hidden” inflammation
1. Brain fog
“Brain fog” is an assortment of symptoms associated with a decline in normal cognitive function. Lethargy, difficulty concentrating, poor memory, and fuzzy thinking are symptoms of brain fog. Per a study published in the journal Frontiers in Neuroscience, inflammation of the brain may be responsible for such symptoms.
What to do:
Luteolin, a flavonoid of the flavone class, is a known neuroprotective agent that serves as a potent anti-inflammatory and anti-oxidant. Widely available as a supplement, luteolin is also found in dried oregano, peppermint, sage, thyme, hot and sweet peppers, radicchio, and celery seeds!
2. Fatigue
While it has been known for some time that inflammation is connected to several severe health conditions, a recent proliferation of medical knowledge “also links chronic inflammation to chronic fatigue syndrome, depression, and general fatigue.” Additionally, “there has been an explosion of recent knowledge of (ways that) inflammation levels can influence your body, brain, and even your behavior” – all factors which contribute to fatigue.
What to do:
As inflammation is likely the primary cause of most cases of chronic fatigue, it is necessary to implement lifestyle changes, including those that have to do with stress, nutrition, and exercise. Supplements such as curcumin, fish oil, ginger, and spirulina may also help.
3. Stomach trouble
The bacteria Helicobacter pylori (H. pylori) affects somewhere between 20 to 50 percent of the U.S. population. H. pylori attack the inner protective coating of the stomach, resulting in an inflammatory response.
Besides bacteria, long-term use of non-steroidal inflammatory drugs – NSAIDs – increases the risk of gastritis, the disintegration of the stomach lining. Aspirin and ibuprofen are the most commonly consumed NSAIDs.
What to do:
Antibiotics designed to neutralize bacteria can treat H. pylori infection. Stoppage of NSAID use will probably cause gastritis to go away. Check with your doctor before stopping any recommended OTCs or prescribed medications.
4. Depression
Inflammation and depression aren’t often mentioned in the same sentence. However, recent research has discovered a probable bridge between immunologic processes and brain mechanisms of depression. (This link also includes other psychiatric conditions.) While depression is not an inflammatory disorder, many studies confirm that inflammation affects the brain chemicals implicated in depression.
What to do:
As with fatigue, lifestyle changes and supplement use is probably the most effective action for reducing inflammation in this case. Cut back on refined sugars, eat more fruits and vegetables, and be sure to get at least 30 minutes of light exercise per day.
5. Swollen or painful joints
Swollen or painful joints are indicative of arthritic symptoms. The most commonly affected areas of the body are the ankles, hands, knees, feet, fingers, and wrists. Rheumatoid arthritis (RA) is distinguishable between other arthritis conditions and symptoms in that it affects the same joints on both sides of the body.
What do to:
If you haven’t already, schedule an appointment with a doctor to check for the presence of arthritis. A comprehensive treatment plan often includes medication and lifestyle changes. Learning how to protect your joints is also beneficial for symptom relief.
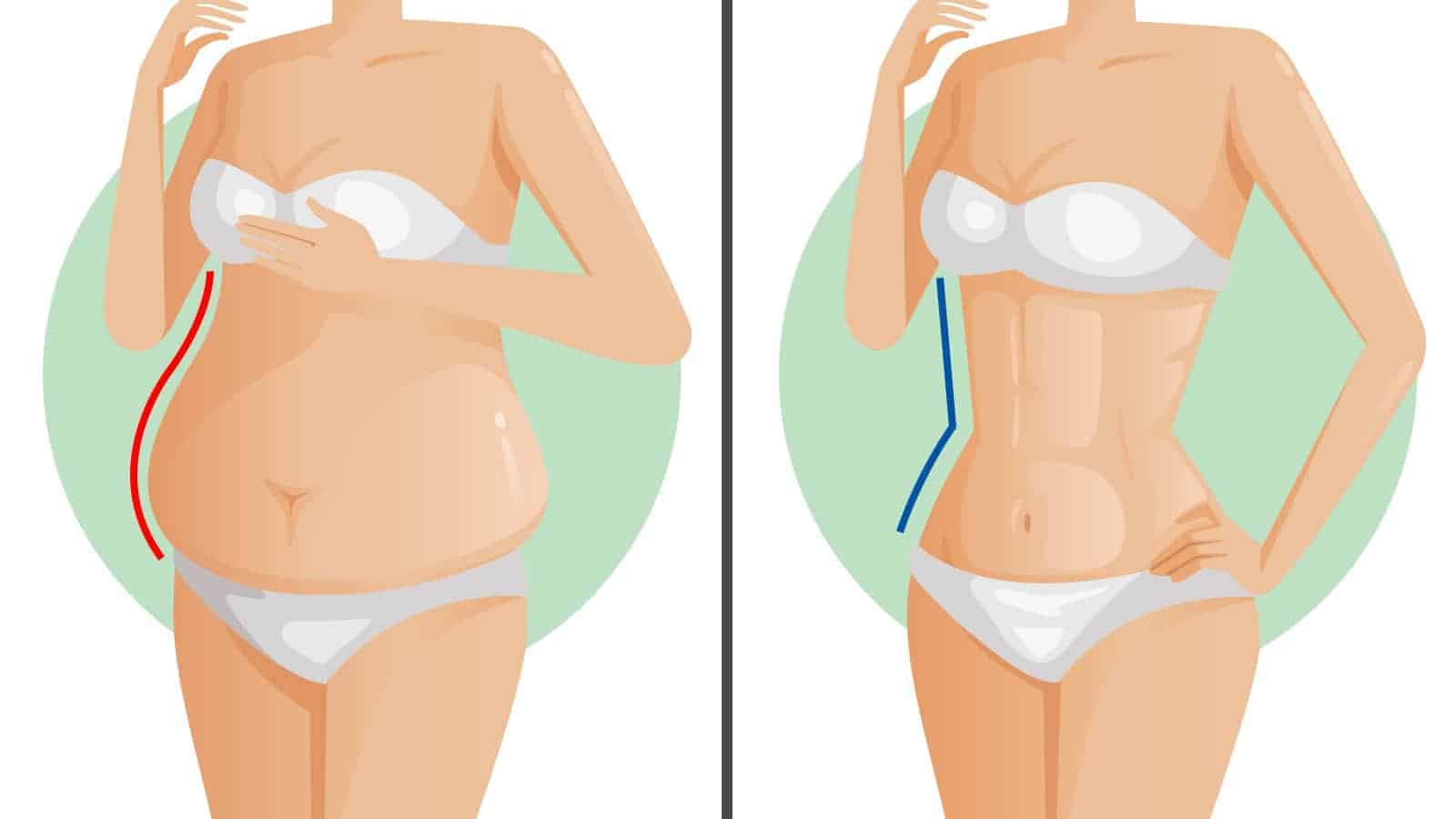
6. Excess belly fat
Per the Washington University School of Medicine, fat surrounding the organs within the gut – also known as visceral fat – secrete inflammation-producing molecules. In 2007, the research team published a study in the journal Diabetes demonstrating that visceral fat contributes to both systemic inflammation and insulin resistance.
What to do:
For many, belly fat is tough to shed – with visceral fat being the hardest. Exercise is likely the best thing for losing visceral fat because fat is used to fuel exercise. Combine a diet of whole grains and fresh fruit and vegetables with a semi-rigorous workout plan. Consider doing some type of HIIT training, such as the Tabata Method.
Gradual weight loss (1-2 pounds per week) should occur. Most importantly, this weight will consist of a healthy share of visceral fat.
7. Red itchy skin
Inflammation is most apparent when it affects the skin. Unfortunately, this happens all too often. Skin that is irritated and red in color may be a sign of either an acute or chronic condition. The former includes conditions like athlete’s foot, dry skin, eczema, insect bites, hives, lice, and ringworm. Long-term conditions producing red, itchy skin include skin cancer, psoriasis, lupus, and various autoimmune disorders.
What to do:
Irritated and red skin should go away on its own; if it doesn’t, see a doctor (particularly if skin symptoms are coupled with other symptoms). In the meantime, keep the affected area clean. Cover the affected area when heading outside. Talk to your doctor about topical creams that may help ease some of the itchiness.
https://www.youtube.com/watch?v=yG-G9_LOkLA












 Community
Community

