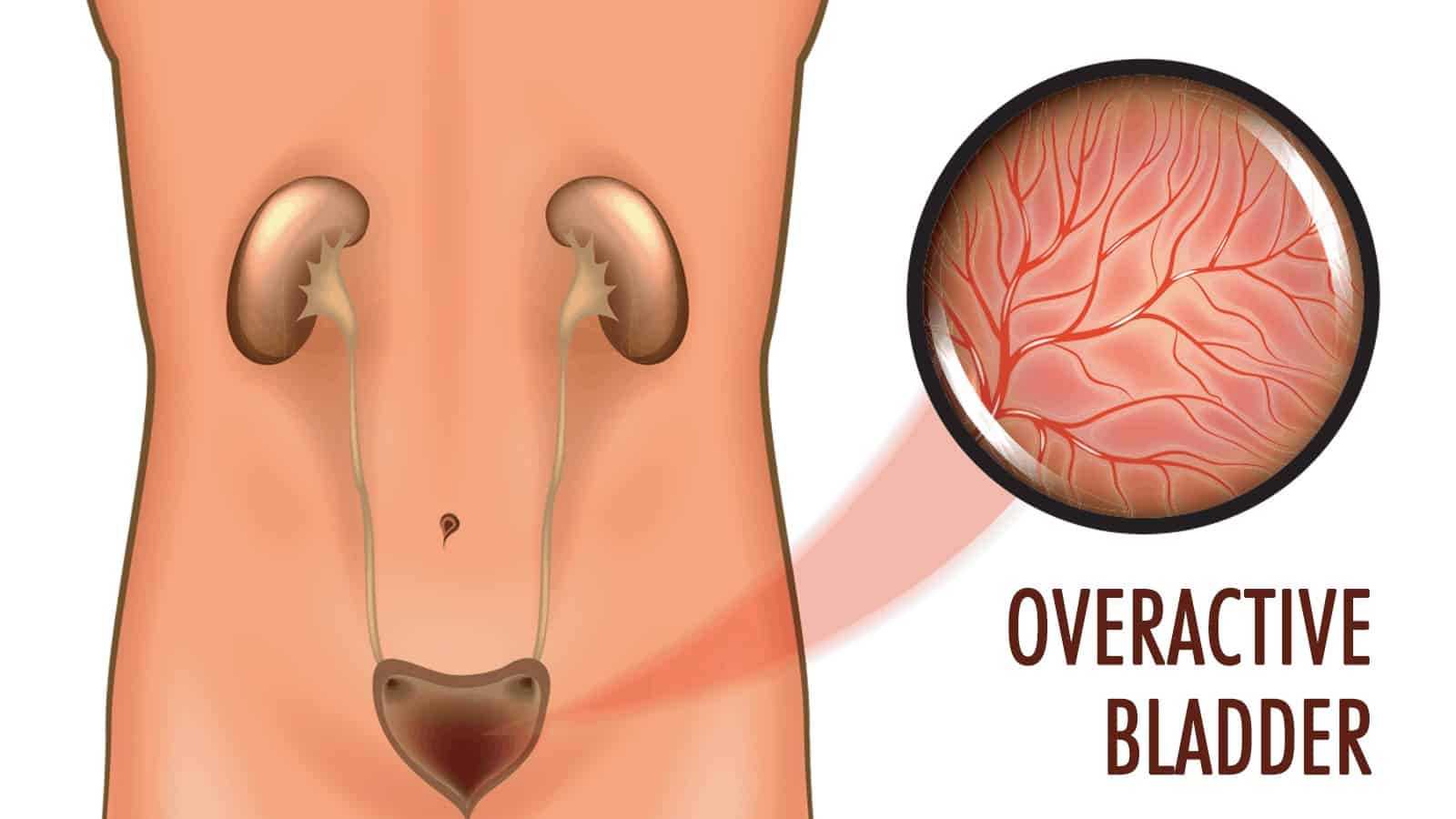
Overactive Bladder (OAB) is a widespread condition affecting millions globally.
According to the Urology Care Foundation, OAB affects over 30 million Americans. This number is likely to be much higher. Counting those who experience intermittent OAB and those who’ve gone undiagnosed, estimates rise to a whopping 30 percent of men and 40 percent of women.
Symptoms and Risk Factors of an Overactive Bladder
Symptoms of OAB include:
- Frequent urination, defined as urinating eight or more times over 24 hours.
- Waking in the middle of the night to pee more than once (a condition known as nocturia).
- Inability to hold your urine.
- Wakefulness.
- Accidental leaking of urine from sudden urges (called incontinence).
The risk factors of OAB are various. They include age-related physical or cognitive decline, neurological diseases such as dementia (e.g. Parkinson’s), and obstruction of the bladder from constipation, enlarged prostate, or surgical complications. They can also be caused by nerve damage to the urinary region, neurological disorders such as multiple sclerosis, stroke, bladder stones, or tumors. Prescription or over-the-counter (OTC) medications that increase the amount of urine production may also be a factor.
Ten Main Causes of Overactive Bladder
It’s important to note that while these are prominent causes, OAB can also result from other conditions or factors not listed here. Always consult a healthcare professional if someone suspects they have OAB.
1. Bladder Fullness
The bladder is a muscular sac located inside the pelvis. It stores urine produced by the kidneys. It stretches to hold urine and contract when it needs emptying. Holding urine for extended periods may seem harmless initially, but it can set the stage for complications.
When individuals consistently delay trips to the bathroom, they train their bladder to hold more urine than it should. This habitual retention can strain the bladder muscles over time.
Moreover, repeatedly clenching the bladder muscles can eventually lead them to become overactive, which can manifest as a frequent and sometimes uncontrollable urge to urinate. This phenomenon only exacerbates OAB symptoms.
2. Diuretics
Diuretics, often called “water pills,” promote kidney urine production. Their primary function is to help the body eliminate excess salt and water.
While diuretics are essential for many patients with heart-related issues or fluid retention, they inevitably increase urine output.
Consequently, individuals on these medications can experience an increase in the frequency of urination, exacerbating or simulating OAB symptoms.
3. Cognitive Decline
The brain and the urinary system are closely interconnected. The brain interprets signals from the bladder and sends messages back to control urination.
This signaling system can get disrupted as cognitive functions decline due to age or specific conditions like MS or stroke. The result? A disconnection in the signals between the brain and the bladder causes unexpected or frequent urges to urinate.
Moreover, other neurological conditions, not just cognitive decline, can also impact bladder control, underscoring the importance of the nervous system in urinary health.
4. Menopause
Menopause is a natural transition in a woman’s life, marking the close of her reproductive years. However, with this change come various hormonal shifts.
Estrogen, a hormone, plays a crucial role in the health and strength of the tissues in the urinary tract. When levels of this hormone decline during menopause, the bladder and urethra muscles can weaken, leading to challenges in holding urine.
Consequently, incontinence or an overactive bladder might become an issue for some women post-menopause.
5. Diabetes or Pre-diabetes
Elevated blood sugar levels characterize diabetes due to the body’s inability to produce or process insulin effectively.
An elevated blood sugar level may cause the kidneys to try to filter and absorb the excess sugar. When they can’t keep up, the body expels the surplus glucose through urine.
This excess glucose in the urine draws more tissue water, leading to increased urine volume. As a result, individuals with diabetes or even pre-diabetes might urinate more frequently, potentially giving rise to OAB symptoms.
6. Urinary Tract Infections (UTIs)
UTIs are infections occurring anywhere in the urinary system: the kidneys, bladder, ureters, or urethra. The most common type of UTI affects the bladder.
A UTI can irritate the bladder, leading to a strong urge to urinate even when the bladder isn’t complete. Some individuals might also experience a burning sensation when urinating, pain, and even cloudy or bloody urine.
While UTIs are treatable with antibiotics, they can exacerbate or simulate OAB symptoms if left unchecked.
7. Bladder Stones
Bladder stones are hard mineral masses that form in the bladder. They can develop when the urine in the bladder becomes concentrated, allowing minerals to crystallize and bind together.
These stones can irritate the bladder lining, leading to symptoms similar to those of OAB. Other symptoms often include pain in the abdomen, blood in the urine, or painful urination.
Treating bladder stones often involves a surgeon removing them.
8. Excessive Caffeine or Alcohol Intake
Both caffeine and alcohol are known diuretics, which can increase urine production and potentially irritate the bladder.
Consuming large amounts of coffee, tea, or alcoholic drinks can stimulate the bladder, leading to a frequent need to urinate.
Moderating or spreading intake throughout the day can help manage these OAB-like symptoms.
9. Medications
Some medications have side effects that may increase urine production or irritate the bladder. That includes certain antihypertensives, antipsychotics, anticholinergics, and over-the-counter cold and allergy medications.
If someone suspects that their medication might be causing OAB symptoms, they should consult their healthcare provider. They might adjust the dosage or switch to a different medication.
10. Neurological Disorders
Other neurological conditions can impact bladder function besides multiple sclerosis (MS) and stroke. Parkinson’s disease, spinal cord injuries, and brain tumors are examples.
These conditions can disrupt the nerve signals involved in bladder control, leading to OAB symptoms.
Preventing and Fixing an Overactive Bladder
Prevention is always the best medicine. With this in mind, let’s first talk about lifestyle choices that lower your risk of an overactive bladder.
The most important factors in preventing OAB are maintaining a healthy weight and getting regular exercise. A healthy body optimizes the functioning of the urinary tract and other vital organs. Further, an active lifestyle is the best way to counteract diabetes and obesity. Other prevention measures include limiting alcohol and caffeine, quitting smoking, and managing any known medical conditions.
Now let’s say you’re struggling with a bit of OAB. Are there measures you can take to counteract it? Many signs point to “yes.” One noteworthy finding reported by Harvard University showed that 70 percent of women who used alternative remedies reported being satisfied with the treatment. These treatments might include supplements, herbs, and therapies.
While research is still a bit sparse (as it often is with alternative treatments), three have shown promise.
Pumpkin seeds.
Pumpkin seeds are rich in omega-3s, which possess anti-inflammatory solid traits. One study found pumpkin seed oil to improve urinary tract function and reduce the symptoms of OAB.
Bladder retraining.
The general idea is to reset your bladder muscles. Eventually, you may get to a point where trips to the bathroom become much less frequent. First, start keeping a journal of how frequently you visit the bathroom. Next, delay your bathroom trips for a few minutes at a time. After a while, this 10 minutes will become a piece of cake, allowing you to hold for 15 minutes, then 20 minutes, and progressively longer.
Kegel exercises.
Kegel exercises (ideally in conjunction with regular exercise) strengthen pelvic floor muscles and limit involuntary contractions. Here’s a rundown of how to do Kegel exercises:
- “Find” your pelvic muscles by cutting off your urine mid-stream.
- Make sure that your bladder is relaxed (read: empty).
- Lie down flat on a comfortable surface. Put your arms comfortably at your sides.
- Relax your butt and tummy area.
- Squeeze your pelvic muscles for about 5 seconds; reduce hold time to 2-3 seconds if it is easier.
- Release your muscles for 10 seconds. Repeat.
- Perform these movements ten times each session. Try doing Kegel’s at least 3-4 times daily.
Final Thoughts on Overactive Bladder
Overactive bladder (OAB) is a condition that affects millions of individuals worldwide, impacting their daily routines, sleep patterns, and overall quality of life. While the frequent and sudden urge to urinate might seem like a minor inconvenience, it can lead to broader emotional and psychological effects, such as anxiety, embarrassment, or even depression.
Understanding the various causes of OAB, as discussed, underscores the fact that it’s not just a standalone condition but often a symptom or side effect of other underlying issues. From neurological disorders to dietary habits, a wide range of factors can contribute to or exacerbate OAB symptoms.
However, it’s crucial to remain hopeful and proactive. With the advancement of medical research, various treatments and management strategies are available, ranging from lifestyle changes to pelvic floor exercises. Moreover, awareness and understanding of OAB are growing, leading to reduced stigma and more open conversations.
Are you experiencing these symptoms? Then contacting a healthcare professional is essential. Early diagnosis and intervention can make a significant difference in managing the condition and improving one’s quality of life.
Lastly, society must support and empathize with individuals dealing with OAB. Compassion and understanding can go a long way in helping someone navigate the challenges of this condition.