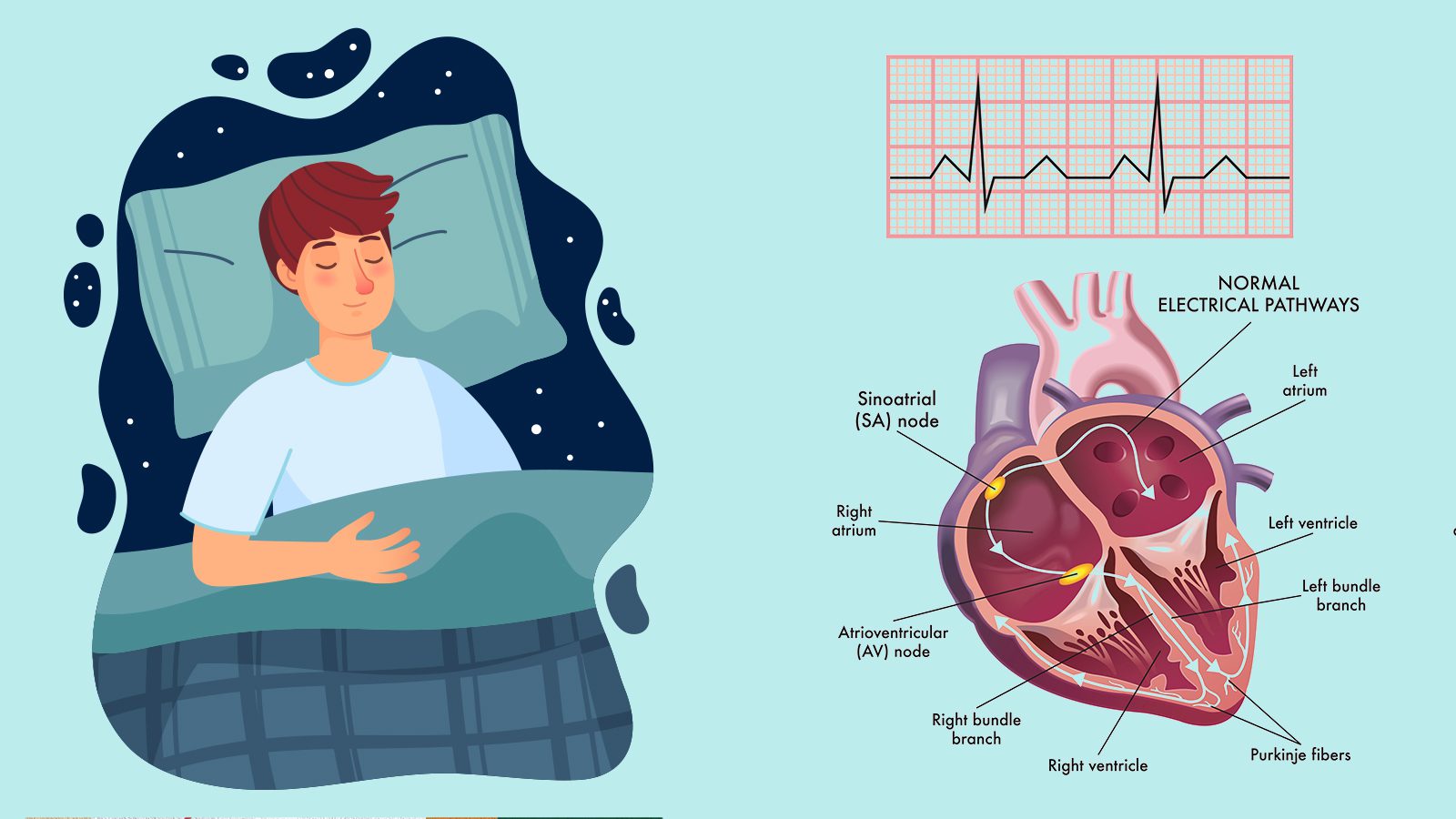
A recent study by the American Heart Association found a link between sleeping soundly and heart health. As a result, they recently updated their checklist to measure cardiovascular health to include sleep quality and duration. Other items on the list include these important heart health and lifestyle factors:
- nicotine exposure
- physical activity
- diet
- weight
- blood glucose
- cholesterol
- blood pressure
Now, the AHA considers sleep essential to optimal brain and heart health. The organization recommends that adults sleep seven to nine hours per night. Children should sleep longer depending on age, they say.
The AHA calls the checklist that measures cardiovascular health Life’s Essential 8™, which replaced the previous Life’s Simple 7™. They published their latest guidelines for heart health in the AHA’s peer-reviewed journal Circulation.
Other Updates to the Heart Health Guidance
The AHA also updated other ideal cardiovascular health measures for people aged two and older. It includes updates on healthy eating habits and exposure to secondhand smoke or nicotine via vaping. Diet guidelines also use non-HDL cholesterol instead of total cholesterol to measure blood lipids. Finally, blood sugar measures include hemoglobin A1c, an important measurement to predict diabetes risk.
Cardiovascular disease remains the leading cause of death in the United States and worldwide. The AHA’s 2022 Heart Disease and Stroke Statistics Update found that around 121.5 million people in the US have hypertension. One hundred million suffer from obesity, while over 28 million have Type 2 diabetes. Additionally, only 25% of adults reported engaging in the recommended levels of exercise, 150 minutes of moderate to intense aerobic activity per week.
However, many studies have discovered that over 80% of cardiovascular disease is preventable. Healthy lifestyle habits such as diet, exercise, and managing other risk factors can stave off risks. Sleeping well also can lower the risk of heart disease, according to the latest findings.
Sleeping Well Promotes Optimal Heart Health
“The new metric of sleep duration reflects the latest research findings: sleep impacts overall health, and people who have healthier sleep patterns manage health factors such as weight, blood pressure, or risk for Type 2 diabetes more effectively,” said American Heart Association President Donald M. Lloyd-Jones, M.D., Sc.M., FAHA, who led the advisory writing group.
He’s also the chair of the department of preventive medicine and the Eileen M. Foell Professor of Heart Research. Additionally, he’s a professor of preventive medicine, medicine, and pediatrics at Northwestern University’s Feinberg School of Medicine in Chicago.
“In addition, advances in ways to measure sleep, such as with wearable devices, now offer people the ability to reliably and routinely monitor their sleep habits at home.”
Over the last 20 years, scientists have made remarkable discoveries on the mind-heart-body connection. As new research came out, the AHA wanted to update its guidelines with the latest information on cardiovascular health. Four of the original metrics have been updated with newer guidelines or compatibility with cutting-edge measurement tools.
The AHA divided their Life’s Essential 8™ elements of ideal cardiovascular health into two categories: health behaviors and health factors. Health behaviors include diet, physical activity, sleep, and nicotine exposure. Heart health factors include BMI, cholesterol, blood sugar, and blood pressure measurements.
“The idea of optimal cardiovascular health is important because it gives people positive goals to work toward at any stage of life.”
“Life’s Simple 7™ has served as a proven, powerful tool for understanding how to achieve healthy aging and ways to improve cardiovascular health while decreasing the risks of developing heart disease and stroke, as well as cancer, dementia, and many other chronic diseases,” he said. “Given the evolving research, it was important to address some limitations to the original metrics, particularly in ways they’ve been applied to people from diverse racial and ethnic populations.”
He added that prior metrics such as diet weren’t as responsive to differences among populations. Also, the guidelines weren’t as sensitive to dietary changes in a single individual over time. So, they decided to delve into the research and refine the metrics to help people improve their heart health. These guidelines can improve many other facets of health as well.
Life’s Essential 8™ Guidelines
- Diet (updated): The new guidelines measure diet quality for adults and children, individually and in the overall population.
- At the population level, dietary assessment stems from consuming foods in the Dietary Approaches to Stop Hypertension (DASH) eating program. The DASH-style diet score includes the following: high intake of fruits, vegetables, nuts and legumes, whole grains, and low-fat dairy. It also contains low sodium, red and processed meats, and sweetened drinks.
- For individuals, the AHA uses the Mediterranean Eating Pattern for Americans (MEPA) to measure cardiovascular health. The MEPA comprises a DASH-style eating pattern assessed with questions about the weekly consumption of certain foods. These include olive oil, vegetables, berries, meat, fish, dairy, grains, etc. However, the questionnaire doesn’t ask about sugary drinks or snacks, so doctors should ask patients during visits.
- Physical activity (no changes): They still recommend 150 minutes of moderate physical activity or more per week for adults. Alternatively, 75 minutes per week of vigorous-intensity physical activity would suffice. Children ages six and older should get at least 420 minutes of exercise per week.
- Nicotine exposure (updated): As e-cigarettes and vape pens have exploded in popularity, the AHA’s guidelines now include these nicotine-delivery systems. Previously, they only monitored the use of traditional cigarettes. Life’s Essential 8™ also measures secondhand smoke exposure for children and adults.
- Sleep duration (new): Optimal sleeping quality and time can improve cardiovascular health. The AHA recommends adults get seven to nine hours of sleep per night. Children ages five and younger should sleep 10-16 hours per night, while those ages 6-12 should get 9-12 hours. Finally, they suggest teens ages 13-18 receive eight to ten hours.
- Body mass index (no changes): The AHA states that BMI 18.5-24.9 supports optimal heart health. However, the writing group acknowledges that healthy BMI can vary among different racial and ethnic backgrounds.
- Blood lipids (updated): They’ve updated the metric for cholesterol to use non-HDL cholesterol as the preferred number to measure, rather than total cholesterol. HDL refers to the “good” cholesterol, while high levels of other cholesterol can increase CVD risk.
- Blood glucose (updated): They’ve updated this guideline to include the option of hemoglobin A1c readings for people with or without Type 1 or Type 2 diabetes or prediabetes. Hemoglobin A1c can measure long-term glucose levels more accurately.
- Blood pressure (no changes): Blood pressure criteria remain the same; the AHA cites a reading of 120/80 or less as optimal.
Final Thoughts on AHA Finding Link Between Sleeping Well and Heart Health
So, in addition to sleeping well, it’s essential to adhere to the other pillars of health. Regular exercise, a healthy diet, keeping your stress low, and managing health conditions can improve your heart health. Also, diet, exercise, and other positive life changes can improve sleep if you have insomnia.
Many people in the modern world suffer from poor sleeping quality, which can affect other aspects of life. However, the AHA reveals why we should all make sleep a priority to restore balance to our minds, bodies, and hearts.